Official data indicate that as many as a quarter of the “ admissions ” of Covid-19 listed by the Ministry of Health may be patients who have contracted the virus in hospital, amid growing questions about how busy the NHS is already over the course of the pandemic.
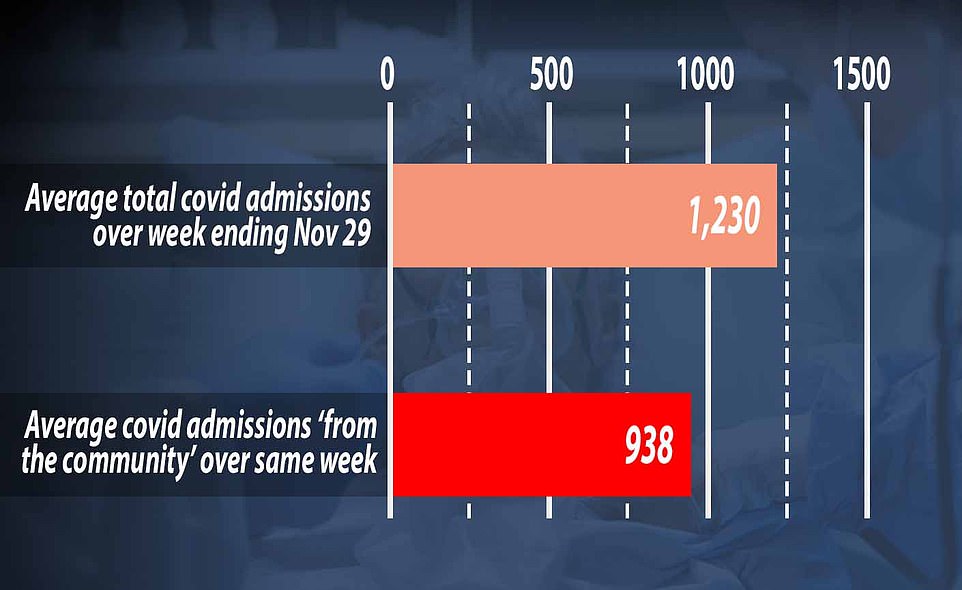
Government figures show there were 1,230 new coronavirus patients requiring NHS treatment daily in England during the week ending November 29 on average.
But only 938 of these – or 76 percent – were accepted by the “ community, ” which means they have definitely contracted the virus in their daily lives.
It leaves question marks over how another 292 admitted patients were infected each day, on average, because the NHS does not detail why they were counted as admissions.
Sources say it was possible that the tests would have been positive after they were admitted for another reason, such as breaking their leg, or they might have contracted the Coronavirus while they were already in the hospital. One official claimed that at least 9 percent of admissions definitely get it in hospital.
Leading experts who have studied the numbers have given similar estimates, including Oxford University professor Karl Heingan who said last month that hospital-acquired coronavirus infections were still “ consistently high ”.
This comes after a whistleblower claimed to The Telegraph that between 17.5 and 25 percent of admissions had contracted the virus in hospital, prompting columnist Alison Pearson to write: “It’s called the dirty NHS.”
Health chiefs have been accused of picking up data to suit their agendas, with critics worrying that the public is being “misled” about the truth in England’s hospitals.
Anger erupted after a MailOnline analysis this week showed that hospitals in England are quieter than usual at this time of year, despite government warnings that health services are on the verge of collapsing.
Government figures show there were 1,230 new coronavirus patients requiring NHS treatment daily in England during the week ending November 29 on average. But only 938 of those – or 76 percent – were accepted by the “ community, ” which means they have definitely contracted the virus in their daily lives. It leaves question marks over how another 292 admitted patients were infected each day, on average, because the NHS does not detail why they were counted as admissions.
In the same telegraph column, “George” – the anonymous source who allegedly sends NHS occupancy numbers every day to the newspaper’s “Planet Normal” podcast – claimed that only a quarter of admissions arrive at the hospital as a confirmed case of Covid.
But the NHS does not publish public statistics about when the admission cases tested positive for the virus, which means that it is impossible to verify them.
An NHS spokesperson said: “ As the National Statistics Office has explained time and time again, when infections in the community are high, NHS staff and patients are more likely to be affected.
“While hospitals are required to follow regularly updated guidelines on infection prevention and control, the best way to reduce hospital infection rates is to reduce them in the wider community.”
Tests are mandatory for patients who go to hospital for all cases, to ensure that infected people do not fly under the radar and lead to an outbreak.
Officials also don’t release figures on how many patients have contracted the virus in hospitals, so it’s not clear how many 292 hospital infections – the technical name for hospital-acquired infections – are.
There is also no data showing whether the admitted patients have already contracted the Coronavirus, or are not showing symptoms but need hospital treatment for something else.
Infection control measures have been tightened during the pandemic to prevent it from occurring, and NHS medical staff are now required to wear protective gear all the time and clean wings and bed sheets periodically.
But transmission of the coronavirus cannot be stopped completely because many people never have symptoms and the tests are not perfect, so they miss some infections.
The numbers support claims about hospital infections from Professor Karl Heneghan’s Evidence-Based Medicine Center at the University of Oxford, which also suggested that up to a quarter of Covid patients develop it in hospital.
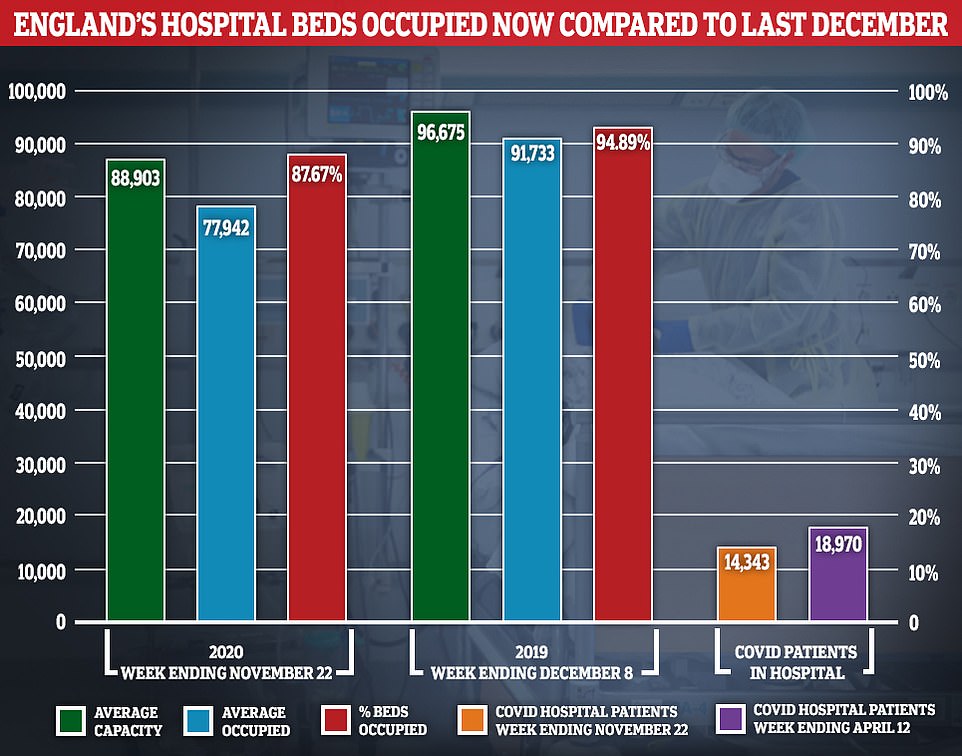
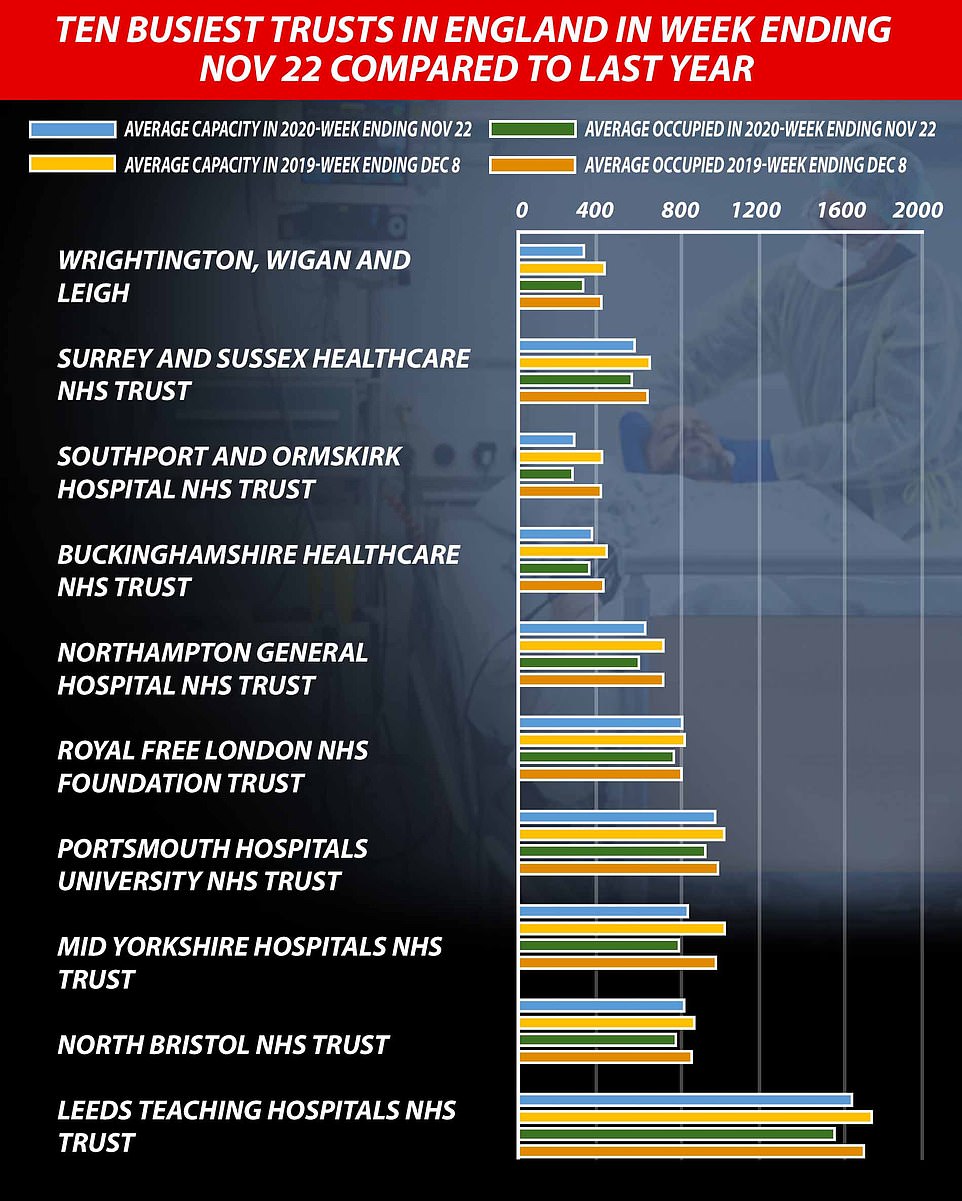
On average, 77,942 of the 88,903 (87.7 percent) households available across the country were filled in the week ending November 22, the most recent snapshot. For comparison, the occupancy rate was 94.9 percent, on average, during the seven-day period ending December 8, 2019 – the most comparable data last winter – when about 91,733 of the 96,675 available beds were full.
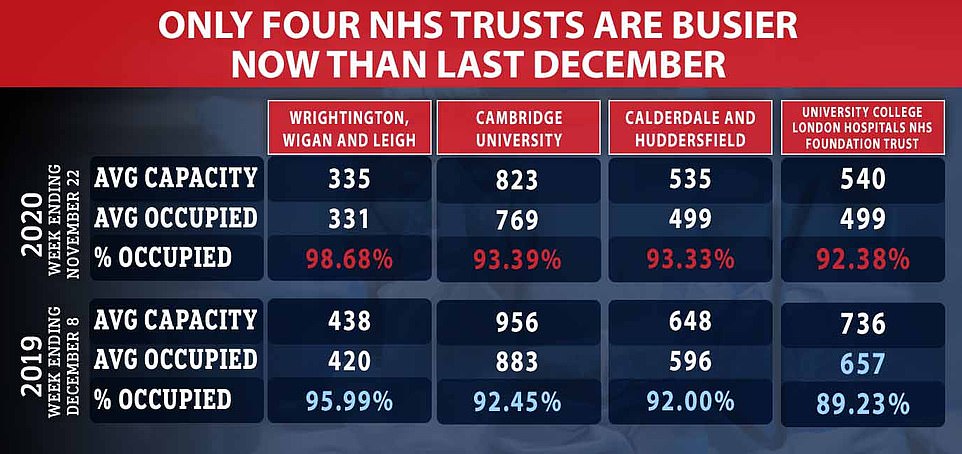
Only four trust institutions – the University of Cambridge Hospitals Foundation (FT), University College London Hospitals, FT, Calderdale and Huddersfield FT, Wrightington, Wigan and LFT – are busier now than they were a year ago
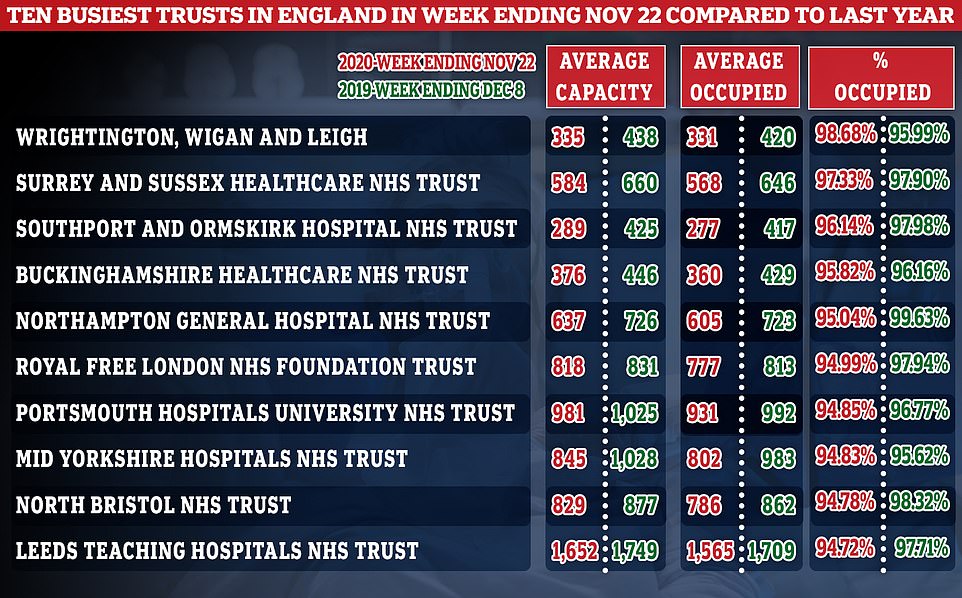
Among the trust funds busiest this year, only Wrightington, Wigan, and Leigh received more patients in total than last winter.
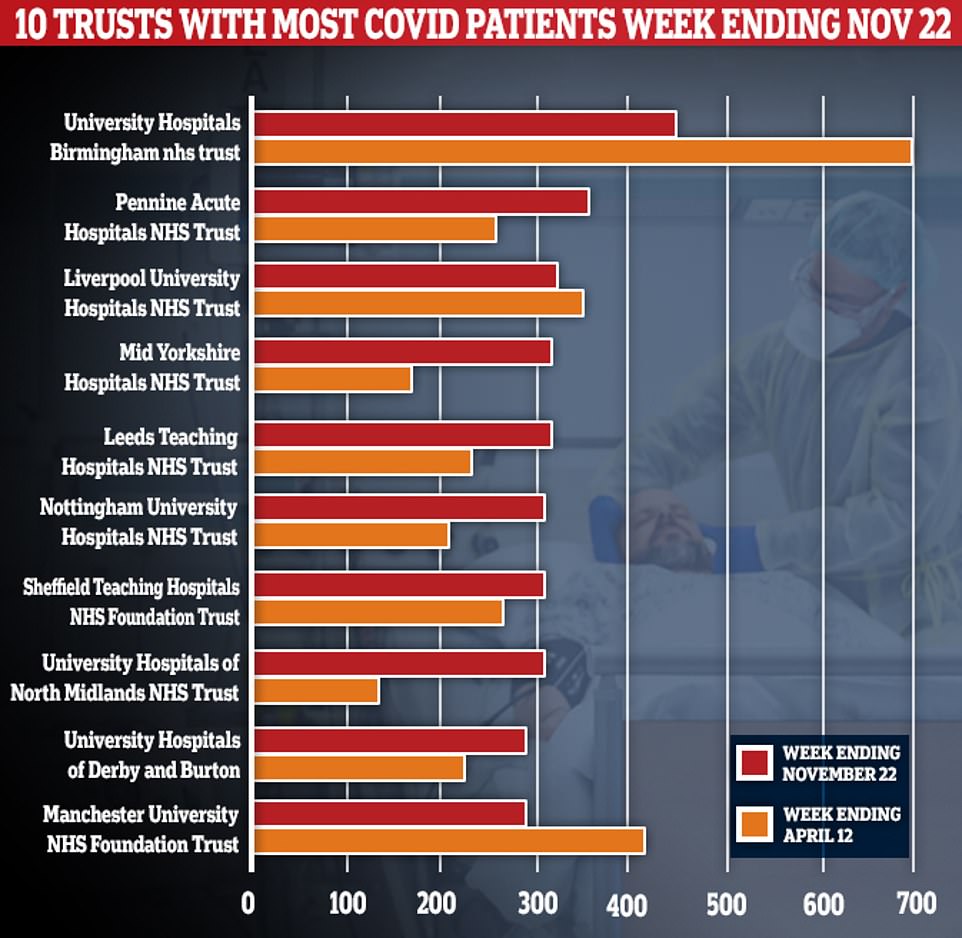
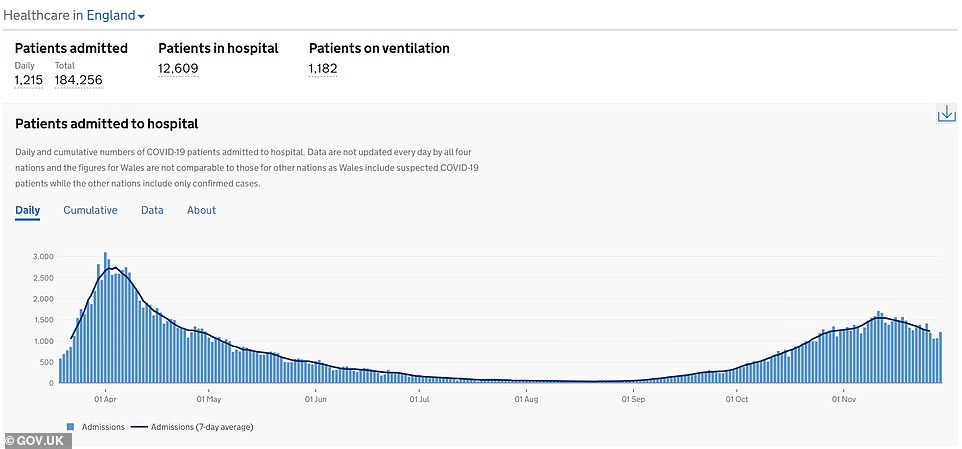
It is true that nearly a third of English hospitals are receiving more coronavirus patients now than they were at the height of the crisis in April. But overall, there are still 4,000 fewer people with the disease in English hospitals than in the darkest days in mid-April.
Experts said at the end of October that about 17.6 per cent of admissions to England had contracted the virus in hospital, and that regional differences had seen as high as 25 per cent in the northwest.
The numbers will add to the growing questions about how accurately the government is recording the impact of the virus.
Officials had to revise the way the deaths were counted over the summer after it emerged that survivors could be classified as victims even if they overcame the disease and were killed in a car accident six months later.
The lack of clarity about how hospitalized coronavirus patients are counted comes at a time when official data appears to contradict public messages spewing doom about the state of the NHS.
Conservative Party Minister Michael Gove said in an article for The Times on Saturday that every hospital in England could be in trouble if MPs do not agree to the revamped three-tier system.
“These new levels, along with the wider deployment of mass testing, have the potential to prevent NHS burnout until vaccines arrive,” he said.
But MailOnline’s analysis of NHS data indicates that hospitals are less full than they were last winter, despite warnings of unsustainable pressure on doctors.
Data show that only four NHS trusts in England – Cambridge University Hospitals Corporation, University College London Hospitals, Calderdale and Huddersfield, Wrightington, Wigan and Lee – are busier now than they were at the same time last year.
On average, 77,942 of the 88,903 (87.7 percent) households available across the country were filled in the week ending November 22, the most recent snapshot.
This number does not take into account the potential for change in a discontinued nightingale or thousands of confiscated beds from the private sector.
For comparison, occupancy was 94.9 percent, on average, during the seven-day period that ended on December 8, 2019 – the most comparable data for last winter – when about 91,733 of the 96,675 available beds were full.
Dr. Carol Sikora, a consultant oncologist and professor of medicine at the University of Buckingham, said Downing Street was running a “brainwashing PR campaign” with “unstacked data.”
He told MailOnline: “We’re back to how I started in March, with [the Government] Allegedly, we need measures to protect the NHS. The data you showed me proves that it does not need protection. He’s dealing with Covid really well.
What the data shows is that hospitals are not operating at full capacity and still have some Covid spare beds if needed. The audience is misled, and the data does not accumulate. Fear and intimidation are used to keep people out of the hospital.
But NHS officials responded to the allegations, with a senior executive saying the national occupancy data “is not a good guide to just how stressful the hospitals are”.
An NHS spokesperson told MailOnline: “ The pandemic has changed the way the NHS delivers care, as hospitals have had to divide services into Covid and non-Covid regions to protect patients in a way that was not necessary less than a year ago, which means some family. They cannot be used due to strengthened infection prevention and control measures.
This means that trying to compare current occupancy numbers to those that were before the pandemic is like comparing apples and pears and does not reflect the real pressures that hospitals are experiencing due to the high numbers of patients infected with Covid-19, which is why. It is important that we all continue to follow government guidelines and help stop the spread of the virus.
The NHS also says: “In general, hospitals will face capacity pressures with lower overall occupancy rates than previously.”
In general, there are still 4,000 fewer people with the disease in English hospitals compared to the darkest days in mid-April.
For comparison, there were 18,970 Covid-19 patients receiving treatment on April 12 – the busiest day since the pandemic began, compared to 14,343, on average, in the week ending November 22.
The total number of hospital admissions – the main measure that includes anyone who has tested positive for the virus – has decreased in England since November 11, not even a week after the country’s second national lockdown was implemented.
But it could take several weeks for people with the disease enough to need an NHS treatment, indicating that the original three-layer system was helping to relieve the pressure on hospitals before the number 10 hit the panic button.

“Music specialist. Pop culture trailblazer. Problem solver. Internet advocate.”